Community Programme For Mental Health



Programme Overview
Our Commitment: To promote healthy lives and the wellbeing of poor and marginalised people at all ages.
Strategic objectives
- To enhance access to holistic mental health services
- To build young people’s resilience against drug and substance abuse
“Breaking Barriers, Restoring Lives: A Community’s Call to Mental Health Action”
Imagine a world where individuals with mental health challenges are not defined by their struggles but empowered by a compassionate community. Join us in making mental health a priority—one step, one smile, and one life at a time.
Focus Areas

To strengthen the communities’ capacity to promote mental health, prevent mental illnesses and care for PLMIs

To support people affected by mental illnesses and drug abuse regain their social, psychological and economic functionalities

Advocate for improved mental health services within WHO dimensions
Projects
Making the invisible visible project (2023-2026)
For years, the Saint Martin Mental Health Programme (Making the invisible visible project) has been a lifeline, bridging the gap between vulnerability and hope. The programme is on a special mission to make visible the different abilities possessed by people living with mental illnesses. People living with mental illnesses should not be defined by their illnesses but by who they have been, and what they remain to be. They are mothers, fathers, children, lawyers, teachers, people with great dream and a promising future. We believe that with the right support, these people can revert to functionality. The programme initiatives transform challenges into recovery and resilient stories. At its heart lies a simple yet powerful mission: to ensure none is left behind on their journey toward mental wellness.
Goal: To strengthen community capacity to promote mental health, prevent mental disorders and care and support people with mental illness.
Interventions
- Identification, screening and assessment of the beneficiaries (people living with mental illnesses) is done with support from volunteers and other community members and clients placed under different programme interventions.
- Counseling: Community Counselling Centre (CCC) is a beacon of hope for those in need of professional guidance and a kind and listening ear. CCC is powered 16 skilled volunteer counselors who offer a safe haven community members can find peace of mind, healing, and renewed hope.
- Treatment support– Depending on the presenting issues beneficiaries are advised to visit the Nyahururu County Referral Hospital Mental Health wing and other health centres for further assessment and treatment. In collaboration with the community, they are assisted to purchase psychiatric medication, payment of health insurance premiums and inpatient rehabilitation in psychiatric wards.
- Capacity building– We believe in empowering communities we train key groups, including: Community volunteers, Family members and caregivers, Law enforcement officers, Local leaders (chiefs, village elders, etc.) and the general publi
- Psychosocial Support: Recovery doesn’t end with treatment; it requires ongoing care, support, and community reintegration. Our psychosocial support intervention ensures that individuals continue to receive the help they need for both clinical and personal recovery through:
- Continuous follow-ups and home visits to monitor progress and provide encouragement.
- Family psycho-education to equip caregivers with the knowledge and skills to support their loved ones.
- Aftercare planning in collaboration with caregivers and volunteers to ensure sustained recovery.
- Livelihood support to help individuals regain independence and stability
Integrated intensive outpatient rehabilitation program (IOP) project
Substance use addiction presents a significant social and public health challenge globally, with an estimated 35 million people suffering from substance use disorders, as reported by the World Health Organization. In Kenya, substance abuse rates remain alarmingly high, with regions like Central Kenya experiencing a notable rise in alcohol and drug dependency, especially among the youth. Despite various rehabilitation efforts, persistent challenges, including social stigmatization, physical, psychological, and emotional difficulties caused by addiction, and
Inadequate community-based interventions hinder recovery. We address this gap through addiction treatment approach and Intensive Outpatient Rehabilitation Programme. This community-based intervention employs a mixed-method approach, integrating the biopsychosocial, 12-step Alcoholics Anonymous (AA), and disease models.
Goal: To enable individuals with problematic substance use, lead productive lives without needing hospitalization or other intensive forms of care.
Interventions
- Identification, screening and assessment of people in level 1 and 2 of the ASAM placement criteria to determine the severity of substance use and appropriate interventions.
- Treatment through a 13-week outpatient programme focusing on group and individual counseling, relapse prevention, behavioral therapies, and skill-building.
- Aftercare phase involves structured follow-ups at home, peer support groups e.g. Alcoholic Anonymous/ Narcotics Anonymous (AA/NA) which happens at St Martin’s grounds every Sunday, relapse prevention strategies, and linkage to educational opportunities through other projects.
- Capacity building- Training of caregivers, peer supporters and volunteers on their support role to enhance recovery outcomes.
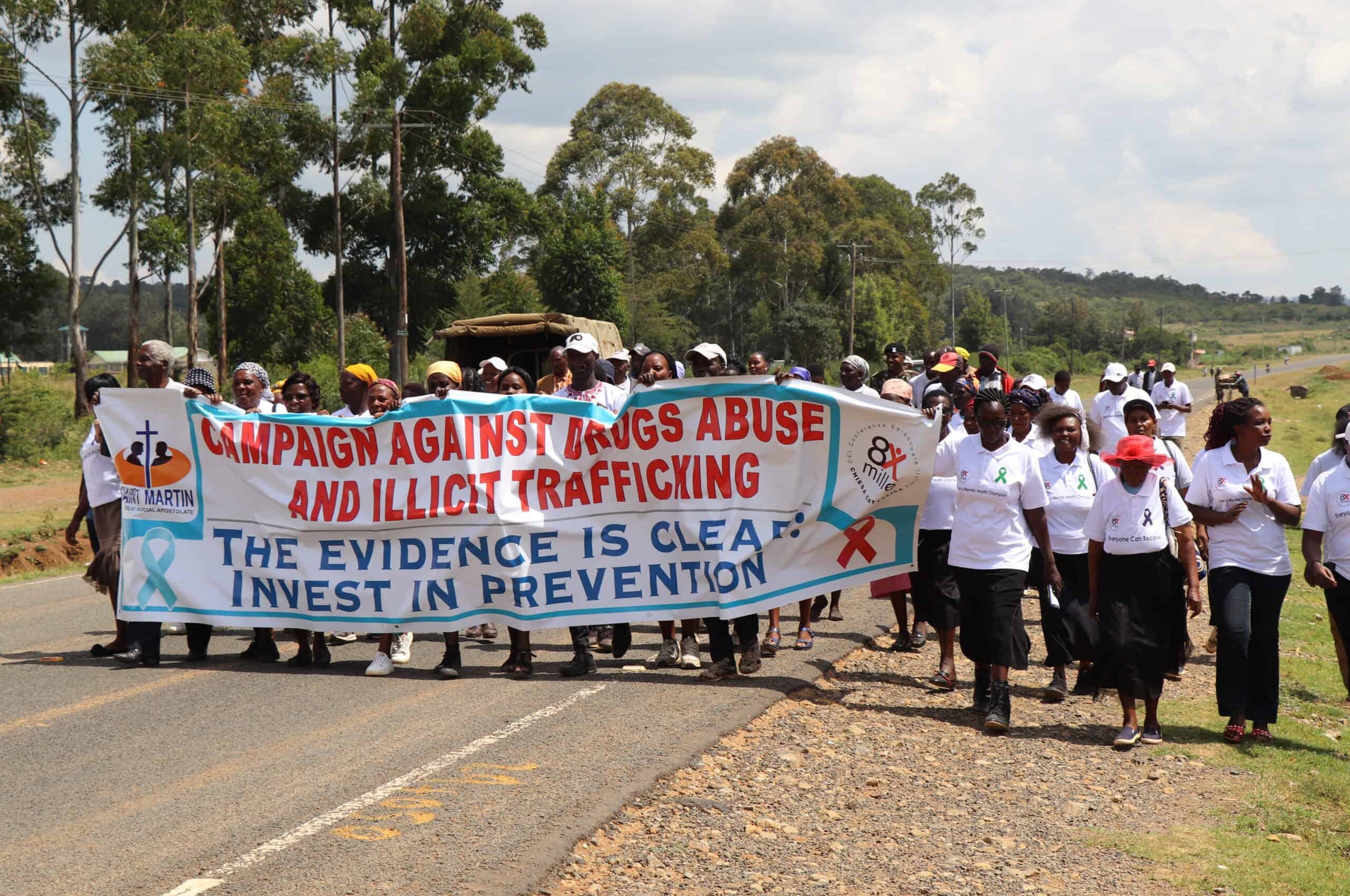
- Community engagement to destigmatize addiction and support people in their recovery journey through awareness campaigns and advocacy.
Promoting alternative approaches in drugs education (PAADE) project (2024-2027)
Substance use and abuse among secondary school students in Nyandarua County has become a growing concern, as evidenced by the increasing number of students seeking counselling services. Over the past three years, St. Martin CSA’s Community Counselling Centre has witnessed a significant rise in referrals related to substance abuse, with over 300 cases recorded in the last one year (2023-2024) alone. This upward trend signals an escalating crisis that may not have been fully acknowledged or addressed within the broader community.
The Ministry of Education, in collaboration with the National Authority for the Campaign Against Alcohol and Drug Abuse (NACADA) and the Teachers Service
Commission (TSC), introduced the National Guidelines for Alcohol and Substance Use Prevention and Management in Basic Education Institutions in 2021. However, despite the presence of these comprehensive guidelines, many school administrators continue to face challenges in effectively managing incidents of substance abuse among students.
Goal: To support effectiveness of school-based drugs prevention programs through evidence-based approaches
Interventions
- Advocating for integration and strengthening of life skills and preventive education in the curriculum
- Retraining guidance and counseling teachers using evidence-based models
- Promoting peer support systems and positive role models in secondary schools
- Advocating a multi-stakeholder collaboration and engagement in preventing and managing alcohol and substance use basic education institutions
- Promoting trauma-informed approaches that focus on understanding and addressing the underlying issues contributing to substance abuse, rather than simply punishing students.





Impact Stories and Testimonials
Achievements and Metrics
Under the Making the Invisible Visible Project, we have;
Get Involved
Help us restore the dignity of people living with mental illnesses

Psychiatric Medication
For many individuals living with mental illness, psychiatric medication is essential to their well-being. It enables them to carry out daily activities and lead fulfilling lives. As one beneficiary shared:
"Without medication, I cannot sleep. This affects my functionality during the day as I am always very tired."
Help us restore sleep, one person at a time.
Donate Ksh 2,000 to provide psychiatric medication for one month to someone in need.
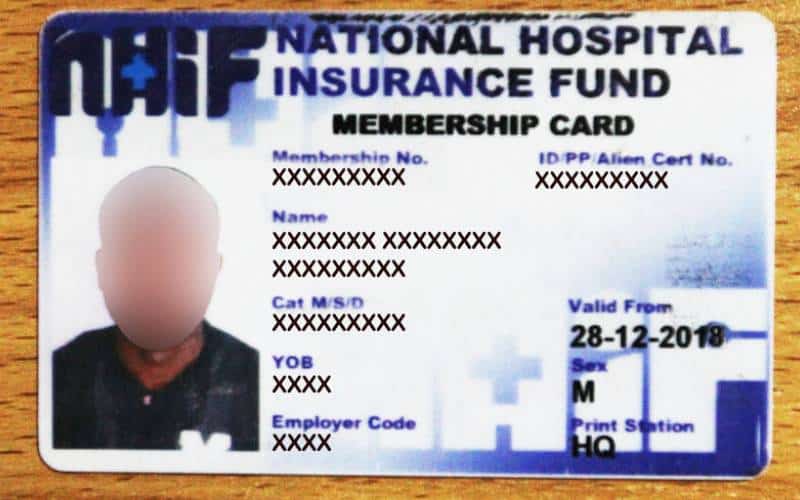
Health Insurance
Health insurance is a critical tool in ensuring access to mental health treatment, especially for inpatient care. It not only covers the person living with mental illness but also extends support to their family, easing financial stress and improving overall well-being.
Benard, a caregiver, shares his experience:
“The insurance cover helped me pay for MRI scan for my wife. I was told to pay Kshs 18000 to cover the cost which I couldn’t afford. However, 1 year insurance payment of Kshs 5400 paid by Saint Martin covered the cost and we will continue using it until one year is over. “Benard, a PLMI caregiver
Donate Ksh. 500 to support 1 person living with mental illness pay health insurance premiums for one month

Emergency Inpatient Care: A Safety Net for Those in Crisis
When mental illness strikes, some individuals lose touch with reality, misplacing important documents, including their insurance details. In such cases, immediate inpatient admission is necessary—but without insurance, they must bear the full hospital bill.
Donate Kshs 2000 to cover the daily inpatient treatment cost for a person in urgent need.

Recovery from Addiction: A Journey of Healing
People in the recovering from drug addiction require support in their journey. Through the 13 weeks program involving interventions like individual and group therapy, recoverees are able to regain their physical and mental health, reunite with their families, participate in social and economic activities and live a full life.
Donate Ksh. 5000 to support one person, recovering from drug addiction go through the Intensive Outpatient Rehabilitation Program in one weekend.
